What if the body you were born into didn’t feel like home — not because of you, but because the world told you it couldn’t be? For trans and gender-diverse people across the globe, gender-affirming care isn’t just about hormones or surgeries — it’s about reclaiming autonomy, healing, and the radical right to exist without justification.
But like most things in a world built on binaries, access to that care isn’t equal. Depending on where you live, who you are, and how you’re perceived, gender-affirming healthcare can be a human right, a legal maze, a distant dream — or a crime.
Welcome to a map of contradiction. This is what care looks like across borders — messy, political, necessary — and the language that helps us name ourselves through it all.
A Global Patchwork of Care
Western Europe
- France: Hormones and surgeries are covered by social security, but access is restricted by psychiatric gatekeeping and hospital waitlists. Advocacy by groups like OUTrans continues to challenge the binary medical model.
- Germany: Offers a “third gender” legal marker (“divers”) and accessible care, but medical transition still involves mandatory psychological assessments.
- UK: The NHS offers gender clinics, but waitlists can stretch over five years. Private care is growing but costly.
North America
- USA: A divided landscape. States like California and New York are trans healthcare sanctuaries, while others like Florida or Texas ban access for minors and criminalize providers.
- Canada: Publicly funded in theory, but varies by province. Indigenous and rural trans folks often face additional barriers.
Latin America
- Argentina: A model for trans rights. The Gender Identity Law (2012) grants legal recognition without medical requirements and ensures access to free gender-affirming healthcare.
- Chile, Uruguay: Making progress with self-ID laws and public healthcare reforms.
- Brazil: Trans surgeries are available in some public hospitals, but discrimination and violence remain rampant.
Asia & Middle East
- Thailand: A hub for gender-affirming surgery (often for Westerners), but local trans people lack legal recognition unless they undergo surgery.
- India: Legally recognizes a third gender, but the Transgender Persons Act of 2019 faces criticism for bureaucratic control and limited protections.
- Iran: Allows (and subsidizes) gender-affirming surgeries, but often coerces individuals into transitioning as a form of “correction.”
Africa
- South Africa: Progressive laws allow legal gender change and offer healthcare access, but the system is slow, underfunded, and inaccessible to many.
- Other regions: In much of the continent, gender-affirming care is nonexistent or actively punished, yet grassroots mutual aid and underground care are growing.
Oceania
- Australia: Legal gender change and healthcare access depend on the state. Parental consent for minors and long waitlists are common barriers.
- New Zealand: Offers state-funded surgeries, but availability is extremely limited — often less than 10 surgeries per year.
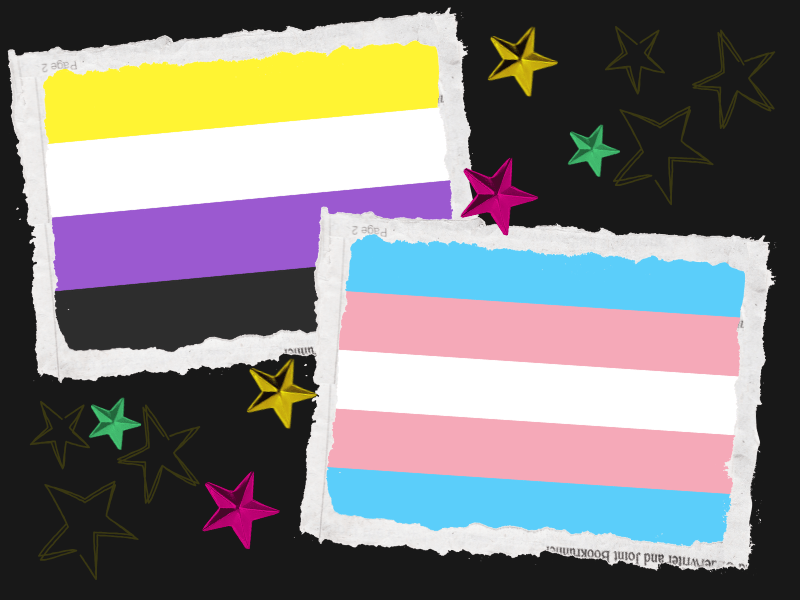
Language Matters: Understanding Trans Lingo
Words are weapons, shields, mirrors. They hold power, and trans people have had to carve our own dictionaries out of necessity and resistance. Here’s a primer — always evolving, never complete.
| Term | Definition |
|---|---|
| Transgender (trans) | Someone whose gender identity does not align with their assigned sex at birth. |
| Cisgender (cis) | Someone whose gender identity aligns with their assigned sex. |
| Non-binary | Any gender identity outside the male/female binary. Includes genderfluid, agender, bigender, etc. |
| Gender Dysphoria | Psychological distress from a mismatch between gender identity and assigned sex. Not all trans people experience it. |
| Transition | The personal, medical, or social journey to live as one’s affirmed gender. |
| Deadname | A trans person’s birth name that they no longer use. Using it is a form of disrespect unless permitted. |
| Misgendering | Referring to someone using incorrect pronouns or gender terms. It’s invalidating and harmful. |
| Top surgery / Bottom surgery | Common terms for chest reconstruction (FTM) or genital reconstruction (MTF, non-binary). |
| Stealth | When a trans person lives without others knowing they are trans — often for safety. |
Q&A: Your Questions, Answered
Q: Do all trans people want surgery or hormones?
A: No. Transition is deeply personal. Some trans people seek medical care, some don’t — and all identities are valid.
Q: Isn’t gender-affirming care dangerous for youth?
A: Absolutely not. Studies show that access to puberty blockers and affirming environments reduces suicide risk, anxiety, and depression in trans youth. Delay or denial of care causes harm.
Q: Can non-binary people access medical transition?
A: Yes. Some non-binary people choose hormones, surgery, or other forms of care to align their body with their gender identity. Medical systems often lag behind in recognizing non-binary needs, but access is growing.
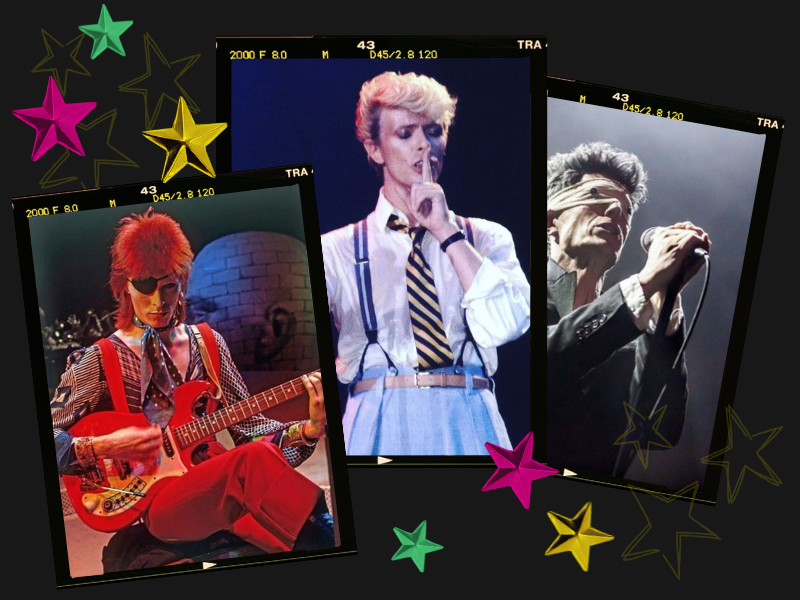
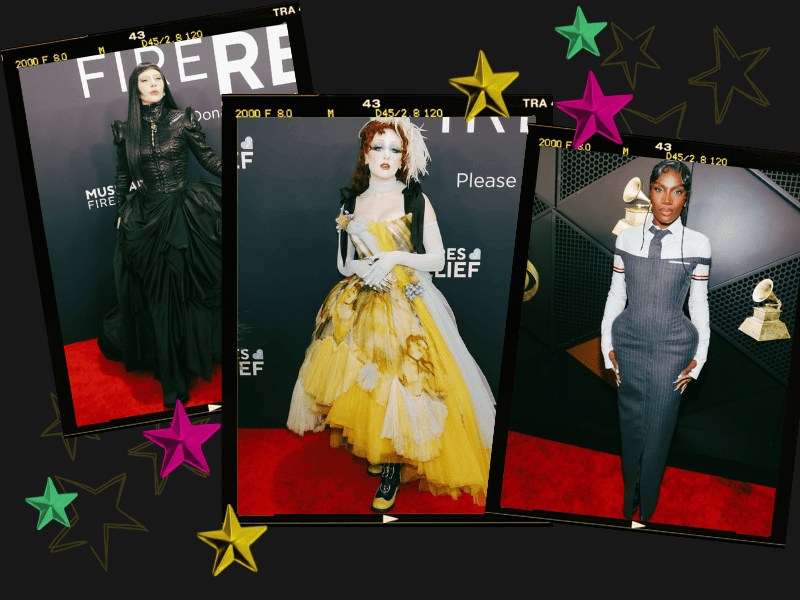
Q: What’s the difference between gender expression and gender identity?
A: Identity is who you are; expression is how you show it. A femme man, a butch woman, and a non-binary person in a suit all defy stereotypes — and none invalidate their gender.
Tips for Surgery (FTM / MTF / Non-Binary)
General tips for all genders:
- Research your surgeon. Look for those with experience in trans healthcare, especially for less common procedures like non-binary top surgery or phalloplasty.
- Be realistic. No surgery is perfect. Set expectations with compassion for your body.
- Know your rights. Some countries require approval letters or “real life experience” — know what your local laws and medical systems demand.
- Plan your recovery. Have a support system, time off work/school, and emotional check-ins in place.
For FTM (female-to-male / transmasculine) people:
- Top surgery: Includes double incision, keyhole, or periareolar techniques. Discuss nipple sensation, scarring, and symmetry with your surgeon.
- Bottom surgery: Options include metoidioplasty and phalloplasty. They vary in complexity, risk, and outcomes — consult multiple professionals.
- HRT (Testosterone): Expect voice deepening, facial hair, increased libido, fat redistribution. Changes are gradual — be patient.
For MTF (male-to-female / transfeminine) people:
- Top surgery: Breast augmentation is optional; some achieve desired growth through HRT alone.
- Bottom surgery: Vaginoplasty, vulvoplasty, or orchiectomy are common options. Healing and dilation require time and support.
- HRT (Estrogen + anti-androgens): Leads to softer skin, breast growth, mood changes, and decreased libido. Effects vary widely.
For Non-Binary people:
- Surgery options: Many opt for gender-affirming procedures without fitting into binary outcomes. Examples: top surgery without hormone therapy, orchiectomy without vaginoplasty, or customized surgeries.
- Medical gatekeeping: Be prepared to advocate for your needs. Not all providers understand non-binary transitions — seek queer-informed care when possible.
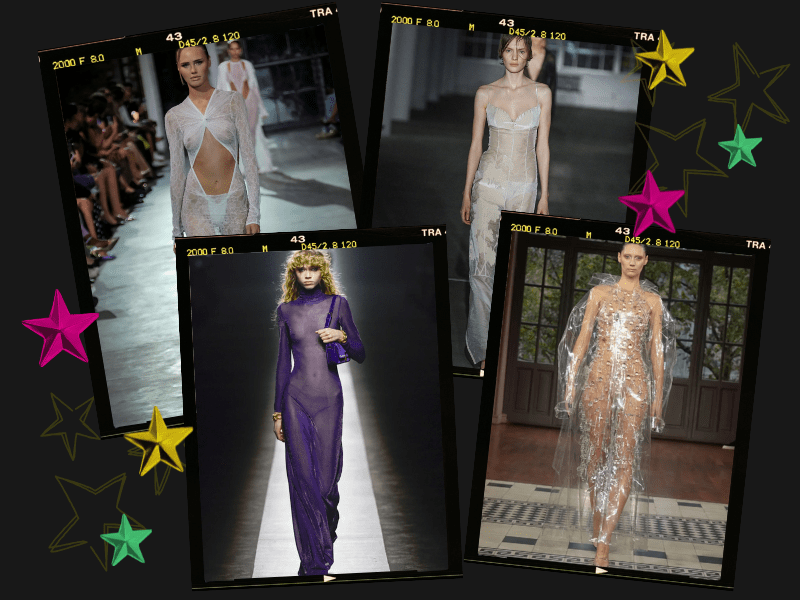
- Voice training & styling: Non-surgical methods like voice work, binding, tucking, or fashion can affirm gender expression meaningfully.
Final Words : Care Is a Right, Not a Privilege
To be trans is not to be broken — it is to break systems that were never built for you.
Trans and non-binary people are fighting, surviving, creating, and healing in every corner of the world. Gender-affirming care is not cosmetic. It’s not luxury. It’s not optional. It is survival. It is joy. It is the basic dignity of choosing how to inhabit your body.
From Buenos Aires to Berlin, Manila to Montréal, the fight is the same: our lives, our voices, our bodies — ours alone.
Let this be a guide, a love letter, and a battle cry.
You are not alone. You never were.


Leave a comment